Welcome to WEEK #6 of the Creative Substitute for “Building Circles of Support!”
Hello Everyone!
Let’s Get Back to Basics: Paradigm Shifting- Bringing it Back to the Brain!
What a strange topic to present after 5 weeks of information and strategies about FASD. Now we are going back to basics???! We got so caught up in the COVID-19 pandemic, that we wanted to provide you with as many strategies as we could to ensure your survival. Although COVID-19 is still with us and we need to keep up diligently with all the great practices of physical distancing and washing our hands, etc., we thought that we would go back to a few foundational facts and ideas about FASD. For many of you, FASD 101 is something you have heard many times, so we will focus more on the parts of the brain which may be affected by alcohol in utero, and how this can often be seen in an individual’s behavior, learning, and development.
- FASD is a medical diagnosis which describes the effects caused by alcohol use during pregnancy. Most often there are no outward signs to show a person has FASD, but parts of the brain are still affected. Prenatal alcohol exposure may affect multiple areas (domains) of brain functioning. The new Canadian Diagnostic Guidelines (2015) require significant impairment (major differences) in at least 3 different areas of the brain resulting from prenatal alcohol exposure before a diagnosis can be made. (Source: The Hidden Disability, New Directions)Individuals who meet diagnostic criteria for FASD may be diagnosed with either:
FASD With Sentinel Facial Features: short palpebral fissures (small eyes), smooth philtrum (smooth skin between the nose and upper lip) and a thin upper lip.
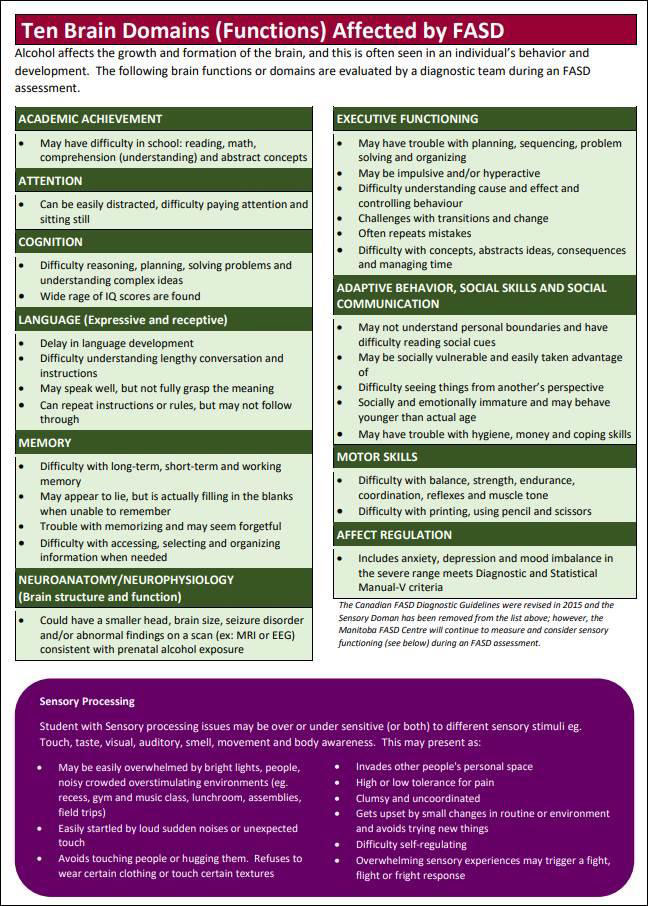
OR FASD Without Sentinel Facial Features: Most individuals receive a diagnosis of FASD without facial features, and they look very typical in their appearance. This is significant because their brain functioning will still be impaired in various ways, and this can have an impact on their behavior, learning, and daily functioning. They are therefore often more “at risk” than the individual diagnosed with FASD with facial features. Therefore FASD is often referred to as the ”Invisible Disability.”The following brain domains are evaluated by a diagnostic team during an FASD assessment:

- This next diagram points out the various behaviors one may see in an individual, if that particular Brain Domain has been affected. It is important for parents and professionals to understand how the affected brain domains are often the underlying reason for the most difficult behaviors of children and adolescents with FASD.
- Watching this You Tube Video by Myles Himmelreich will give you an idea of how brain differences in FASD can have an impact on behavior and learning. He also points out that FASD might not only affect the brain, but rather needs to be seen as a Whole Body Diagnosis. He talks about the results of a Health Survey of 500+ adults diagnosed with FASD, and how people with FASD experienced physical health problems at a rate much higher than the general population.
- Diane Malbin, an expert of FASD and brain based behavior, suggests that since often the individual with FASD’s behavior is a result of brain “differences”, this warrants a different approach to managing the individual’s behavior. When we “reframe a behavior” and shift from seeing an individual with FASD as one who won’t do something (defiant, deliberate, non-compliant, aggressive behavior ), to one who possibly can’t due to brain differences, we shift from personal feeling of hopelessness, anger, and confusion, to one of understanding and hope. This should lead us to “Trying Differently and Not Harder”.
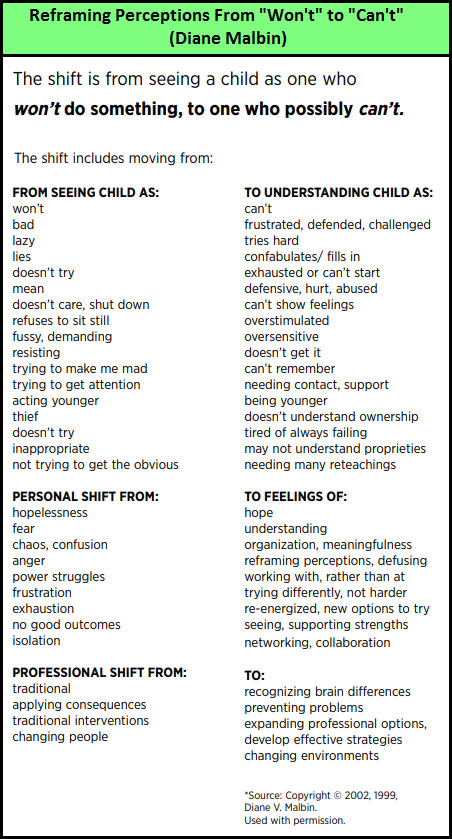
“Beliefs dictate behaviors. The belief that many primary learning and behavioral characteristics associated with FASD are the result of willful, volitional, or intentional behaviors often leads to a punitive approach to the symptoms. The key…. Is linking the idea of brain functions with presenting behaviors, reframing perceptions and moving from punishment to support.” (Source: Healthy Child Manitoba: What Educators Need to know about FASD)In this video: Fetal Alcohol/Neurobehavioural Conditions: A Brief Introduction to a Brain Based Approach, Diane Malbin does a great job of bringing this point across. She presents us with a brief Introduction to a “brain based” or “Neurobehavioral approach” for understanding and working with individuals with FASD and other neurobehavioural conditions more effectively. It is worth taking a look at this video. - Additionally check out the “This is Me” Website and look at reframing the behaviors which are often seen when a specific brain domain is affected. After you view the scenario, try coming up with a brain based approach for intervention rather than a “punitive” one (e.g. time out, withdrawal of privileges, reward system). For those of you with adolescents with FASD at home, invite them into viewing these scenarios with you. After all… they are the experts and they can often give you the best input for “Trying Differently”.
- “My Brain, Me and FASD” is an Interactive Booklet for children and adolescents with FASD to help them understand their brains better. This can be a very powerful tool to help reduce stigma around FASD and help the child start seeing themselves in a more positive way.